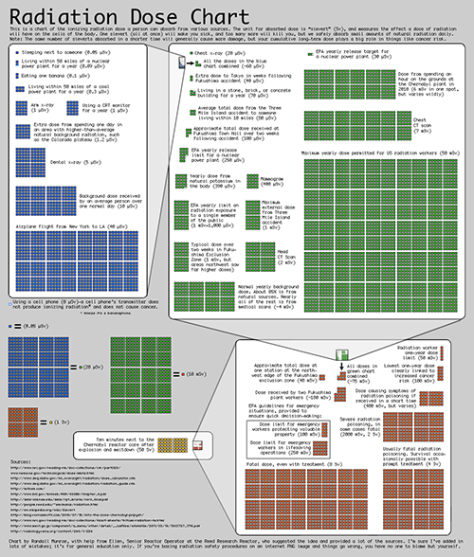
Even though it is something carried out in hospitals hundreds of times a day, X-rays and CT (computed topography) scans are procedures that expose the patient to radiation. Yes, the radiation dosage for the majority of scans carried out is very little when compared to every day exposure; for example an X-ray of the arm is 0.001 mSv (millisievert), a dental X-ray is 0.005 mSv, a chest X-ray is 0.020 mSv – in comparison the average background radiation received over one day is 0.010 mSV, while someone flying across the continental USA would receive 0.040 mSV. However, other scans are higher, a mammogram is 0.400 mSv (equivalent of 40 days worth of exposure in one dose), while a head CT scan gives a dose of 2 mSv (equivalent to ~7 months) and a chest CT scan 7 mSv (equivalent to ~20 months) (see the below image from Randall Munroe for more examples).
Although the cells in our body are able to repair and restore DNA damage resulting from radiation, the greater the dose received in one go, and the greater received in the long-term, the more likely it is that damage won’t be repaired correctly. Thus, we should aim to reduce patients’ exposure to radiation where possible. A recent paper by Kitchen and colleagues may have an answer by using phase-contrast x-ray imaging.[1] Because soft tissue has similar X-ray absorption properties to bone, which results in poor image contrast the radiation dosage has to be increased in standard scans. This new technique combines CT scans with phase retrieval and an algorithm to define edges, densities, etc. and results in a reduction in dosage by a factor of 300 fold (with the potential for a reduction factor in the tens of thousands), while still retaining equivalent image quality. Although the study only tested this in an animal model it is an important first step.
— Peter Chilton, Research Fellow
- Kitchen MJ, Buckley GA, Gureyev TE, et al. CT dose reduction factors in the thousands using X-ray phase contrast. Sci Rep. 2017; 7: 15953.